Multiple Sclerosis (MS): When Does The “Great imitator” Become End Stage?
 Most healthcare professionals have had experience dealing with patients with Multiple Sclerosis (MS) at some point in their career. Some may even have a personal connection to this mysterious disease. I, unfortunately, have experienced both.
Most healthcare professionals have had experience dealing with patients with Multiple Sclerosis (MS) at some point in their career. Some may even have a personal connection to this mysterious disease. I, unfortunately, have experienced both.
As a 19-plus-year hospice nurse, I've cared for more than my fair share of patients with MS. Most fought a valiant battle against this disease. Some actually conquered the symptoms of the disease, even if only temporarily.
Let me start from the beginning and try to explain a little about this disease. MS is a disease of the central nervous system. Some researchers believe that MS is an autoimmune disease, much like Lupus. MS is a tricky, sneaky disease that can mimic other diseases. In fact, as with Lupus, some call it the “Great Imitator.”
For example, there are many diseases commonly mistaken for MS including Myasthenia Gravis, Lyme’s disease, Stroke, Fibromyalgia, acute disseminated encephalomyelitis (ADEM), Sjogren’s syndrome, Vasculitis, Sarcoidosis, Vitamin B Deficiency, Neurosyphilis, Binswanger’s disease and Systemic Lupus.
MS Symptoms
Symptoms commonly seen in these diseases are the same symptoms that an individual with MS may experience -- making it a long and hard diagnosis progress. Symptoms can include:
-
Blurred or double vision --This symptomis commonly seen and reported as a “first symptom” of the disease.
-
Numbness -- This is fairly common and may be one of the first symptoms that causes an individual to seek out medical advice.
-
Fatigue -- Another common -- and life altering --symptom is fatigue. Approximately 80 percent of all patients with MS suffer from various degrees of fatigue. Many experience a severe level that only progresses as the day advances. It can be an all-encompassing, indescribable fatigue. The individual may find it difficult to even lift their arm or walk to the bathroom without extreme exhaustion.
-
Difficulty with balance and coordination -- This is a hallmark symptom of MS. The cause seems to be triggered by impaired nerve conduction. It means that the muscles are not responding appropriately and therefore, the individual may feel weakness in one limb. They may demonstrate a stumbling gait or may constantly experience issues with dropping items. It can be terrifying for the patient.
-
Pain -- This devastating symptom requires aggressive intervention. Most patients with MS will have various degrees of pain such as severe burning in the extremities. It could be a searing, stabbing pain because the nerves are inflamed. It can impair the individual’s ability to sleep.
-
Cognitive dysfunction -- This frightening symptom is common. In fact, studies state that it can affect up to 60 percent of all MS patients.
There are many other symptoms, including heat sensitivity, muscle spasticity, bladder dysfunction, constipation, depression, anxiety, speech impairment and vision impairment.
Learn about the hospice eligibility criteria for MS.
MS Diagnosis and Progression
Due to the multitude of symptoms and possible diseases, obtaining an accurate diagnosis can not only be exhausting for the individual, but frustrating too. At times they’re labeled as a hypochondriac, implying that they’re obsessed with the idea of having a serious disease. In some cases, it can take years to definitively confirm (or rule out) MS as the diagnosis.
Most individuals will experience their first set of symptoms anywhere from their twenties to their forties. Alarmingly, MS affects from 250,000 to 350,000 people in the US and up to 2.5 million worldwide. The reason it’s so difficult to diagnosis is there are no clear cut diagnostic tests that confirm or deny the disease, although Magnetic Resonance Imaging (MRI) has improved the diagnostic process. Typically the disease is diagnosed by process of elimination, ruling out what it is not.
The progression of the disease is as varied as the diseases it mimics. There are three types of MS.
-
Relapsing-Remitting MS (RRMS) -- The most common form. The symptoms appear for a period of time and then remit.
-
Primary-Progressive MS (PPMS) -- In this form, the symptoms worsen because the “remitting” phases are less frequent and are much shorter in duration.
-
Secondary-Progressive MS (SPMS) -- This type of MS begins with a Relapsing-Remitting course of the disease and is followed by the Primary-Progressive course.
Role of Gender and Age in MS
One of the many mysteries of MS is the different way it affects different people, specifically when it comes to gender and age. MS doesn’t affect one gender or age group more than the other, but from what’s known the type of MS and the age of the onset have been correlated with the gender group it affects.
PPMS varies according to the age of the individual. Under the age of 30, it affects an equal number of men and women. At 45 or older, women are affected more than men. After age 50, women are affected at a rate of almost two to one compared to men.
When it comes to the severity of the disease, it’s been determined that men with PPMS usually experience more severe symptoms than women. Large studies show that early on, PPMS in men and women had equal disease severity and rates of progression. Yet, 20 years post-prognosis, men with PPMS began to supersede women with PPMS in severity.
When you look at all types of MS, women outnumbered men at a ratio of three to one when developed before the age of 20. Currently, twice as many women are living with MS. Unfortunately, the rate is dramatically increasing. Some estimates show that the number is steadily rising and is currently at a ratio of four to one and is not slowing.
The Role of a Hospice Nurse in MS
So where do I fit in as a hospice nurse? Hospice nurses usually become involved with an MS patient when the patient and family determine that the symptoms are too hard to palliate. They no longer want frequent trips to the hospital, ER and long hours in the physician’s office.
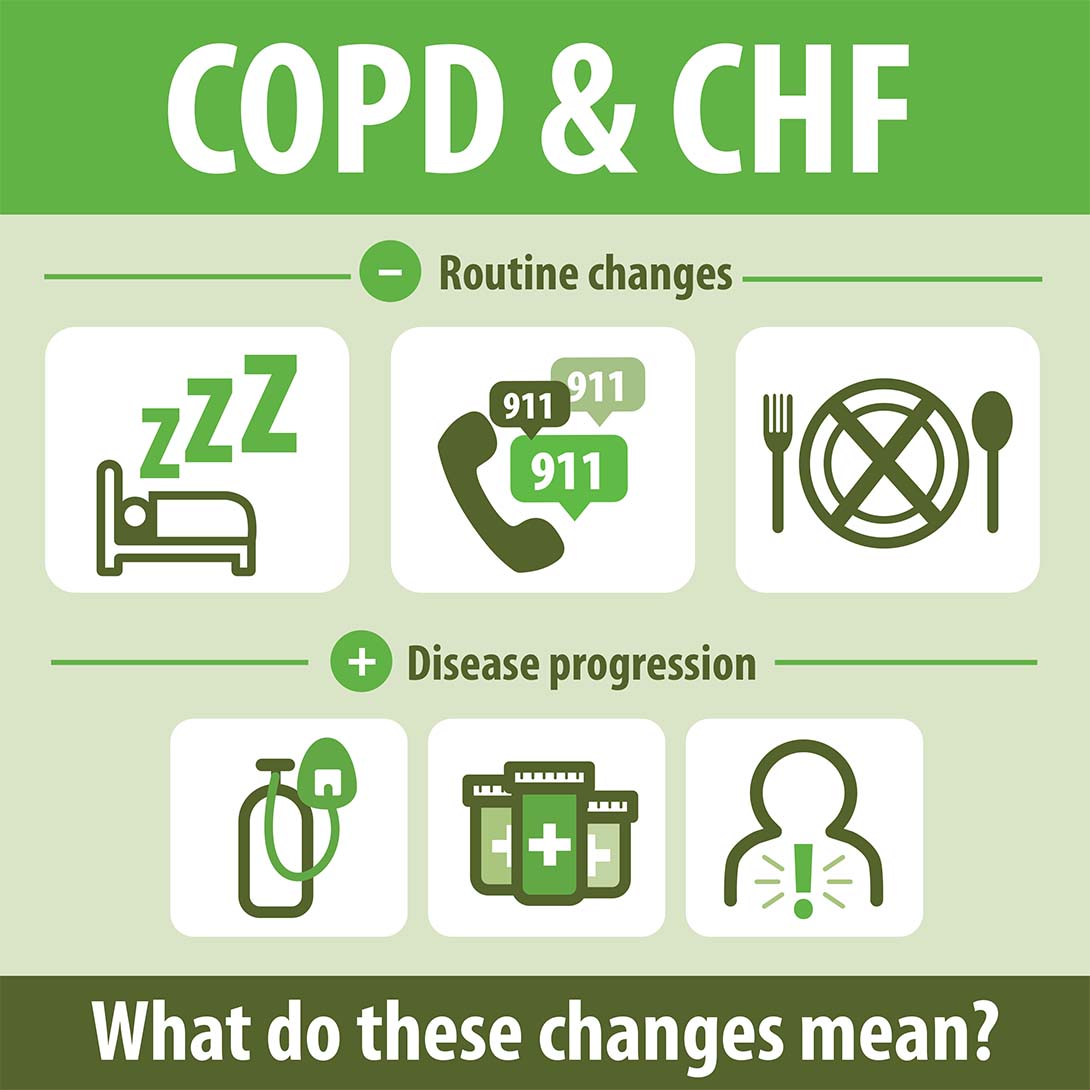
Physically and clinically, the patient begins to experience more pronounced complications from the disease, including a deteriorating respiratory function as well as increased respiratory secretions. The patient may eventually lose the ability to feed themselves or to swallow. They may experience significant weight loss due to the nutritional complications. This may include dysphagia, choking and at times, aspiration.
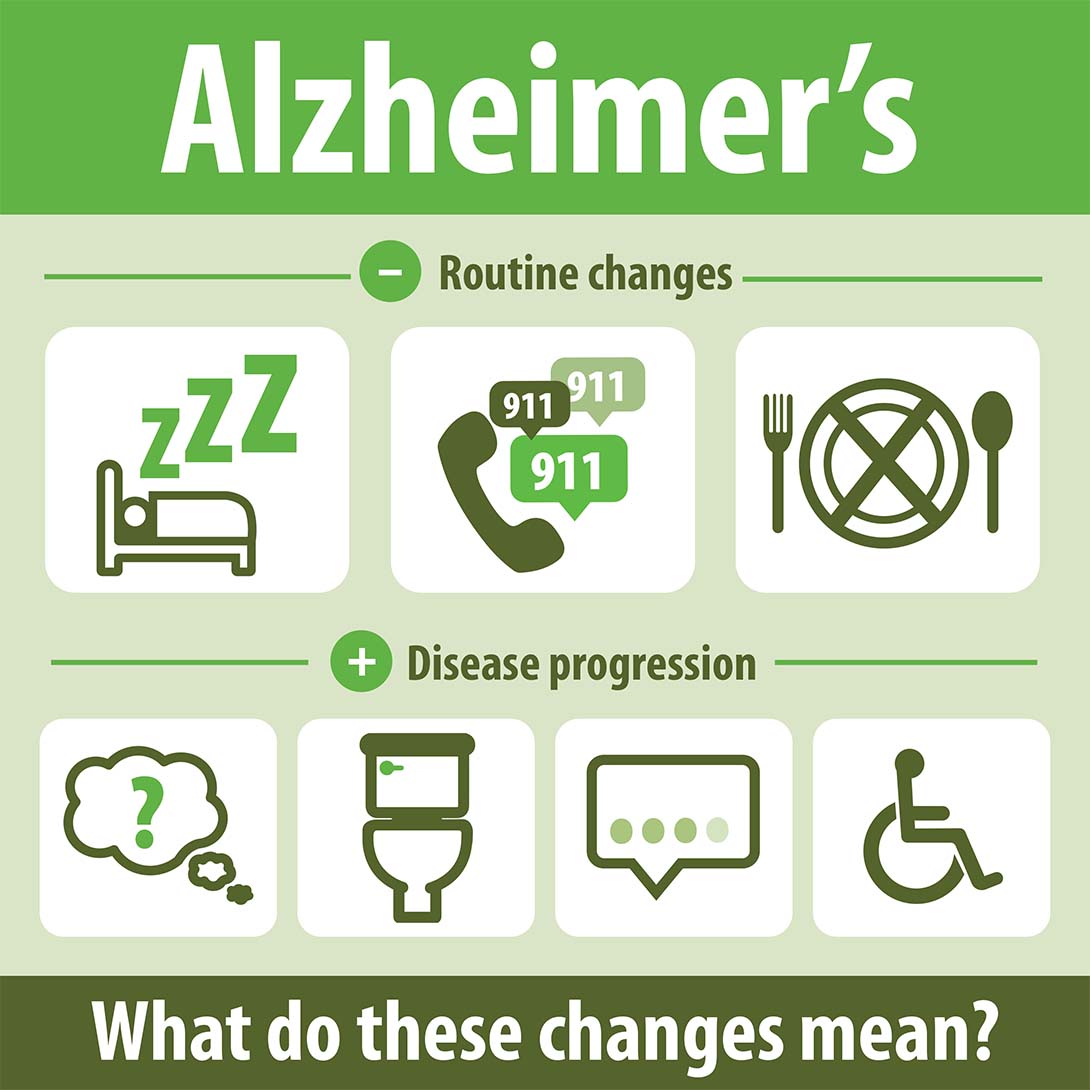
With the significant changes in the patient’s condition, hospice care at this time can offer the patient aggressive symptom management to ensure their quality of life is maintained to the highest standard possible. It also offers emotional support to their loved ones. Some of the complications that affect the patient, and ultimately caregivers and loved ones, as time progresses could include:
-
Pain -- This typically becomes more severe and harder to manage as time goes on. The pain is more complex and may require different types of pain management techniques to ensure that the patient is comfortable.
-
Speech -- The patient has a more difficult time verbalizing their needs, wishes or concerns.
-
Neurological deterioration -- This complication is more pervasive. Mental status changes are more pronounced along with obvious changes in brain function. Some actually experience mood swings and depression.
-
Mobility -- The patient’s ability to move is profoundly affected, and they can even lose the ability to ambulate. They may become bed-bound and may lose the ability to reposition themselves from one side to another.
-
Skin breakdown, severe decubitus ulcers and muscle atrophy -- Limited mobility, in conjunction with the nutritional compromise, leads to these complications.
-
Muscle spasms and tremors -- This becomes more common as the disease progresses.
As with most diseases, MS symptoms are as unique as the patient with the disease. Hospice staff are equipped with the skills and experience needed to help a patient cope with the ever-changing complications.
Unfortunately, there is no cure for MS. The goal is to slow the progression of the disease and improve the patient’s quality of life for as long as possible.
Oh, and as far as my personal connection? I was diagnosed with Systemic Lupus after years of ruling out other diseases and given the tentative diagnosis of MS. I can relate -- to a small degree -- with those patients who experienced the fear of being diagnosed with this debilitating disease.
DeAnna Looper RN, CHPN, CHPCA
Crossroads Hospice
Senior Vice President of Clinical Operations
For additional information on how Crossroads Hospice supports those with MS, please contact us now, or call 888-564-3405.
If you found this information helpful, please share it with your network and community.
Copyright © 2015 Crossroads Hospice. All rights reserved.