How to Live Your Best Life with a Chronic Illness

“It is not length of life, but depth of life that matters.” – Ralph Waldo Emerson
Coming to terms with a serious illness diagnosis can be difficult.
The realization that one will be dealing with a number of new and likely progressive restrictions can be disconcerting, if not depressing. Not being able to participate in or enjoy as many activities as before, requisite changes in lifestyle or nutrition, limits on one’s mobility or ability to work or to travel all can weigh heavily on the mind.
Recognizing what is happening and understanding what to expect are important in making decisions about the course of action you, your doctor, and the rest of your caregiver team decide upon – and in understanding how palliative care can support that strategy, allowing you to live your best life with a chronic illness.
Stress and Depression
Stress and depression can be frequent co-travelers for people living with a chronic illness. It’s not hard to understand why. The reality of serious illness is often accompanied by very real fears and anxieties – uncertainty about the future, fear of long-term disability, financial uncertainties, and more.
Patients should understand that being angry or feeling sad about what is taking place is natural. They are also signs of stress. Losing interest in activities that you once enjoyed is another tell-tale sign. Don’t be afraid to ask a doctor or a counselor about possible warning signs of depression.

Self-Help
You can also try making contact with a local support group where there is a chance to meet and talk with other people who have been through what you are experiencing and maybe give you advice, companionship, or links to other resources.
In addition, trained counselors may be able provide some tools for dealing with many of the emotional challenges that a serious illness poses, not only to the patient, but also his or her loved ones.
In that same vein, be sure to make time for family and friends and focus on those relationships that are most important. These, after all, are the people who have known you the longest, best understand you, and want to look out for your welfare. Maintaining strong, positive social ties is vital to living your best life with a chronic illness.

Communication is Key
For many people facing chronic illness, information is the best medicine. The more you know and understand about your own body and what is happening, the better prepared you will be to understand treatment options – including palliative care, to help manage any pain and discomfort.
Patients often rely on their primary care doctor to lead the conversation about prognosis and treatment options (a fact that Medicare recognized two years ago by the initiation of new billing codes in support of physician-directed advanced planning discussions).
But as Dr. Timothy Ihrig, Chief Medical Officer for Crossroads Hospice & Palliative Care notes, prognosis and treatment should not be the beginning and end of the conversation.

Treating the Whole Patient
“It’s important for medical professionals to try to understand the totality of the patient as an individual,” Dr. Ihrig says. “Our goal should be to help them find a way to live lives that are as full and fulfilling as possible.”
That begins with communication. What kind of quality of life can the patient look forward to? If their illness is life-limiting, how do they want to spend their remaining time? What is most important to them? Spending quality time with family or friends?
“As medical professionals, we need to understand our patients’ concerns as well as their goals in life, so we can help them make decisions that are right for them,” he says. That could mean having discussions that that go beyond potential curative treatments, including palliative care options designed to minimize pain and discomfort that will enable the patient to enjoy an enhanced quality of life for as long as possible.


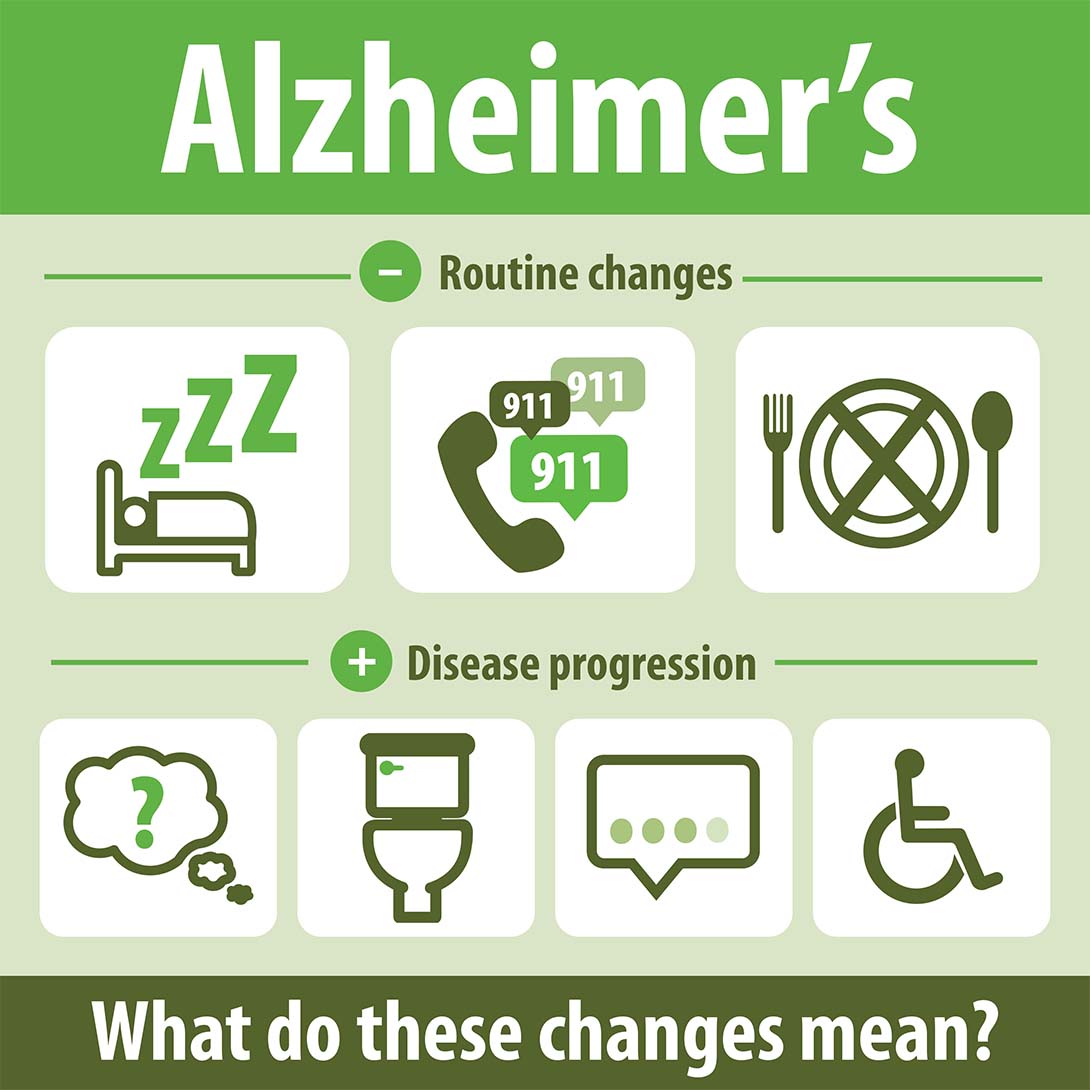
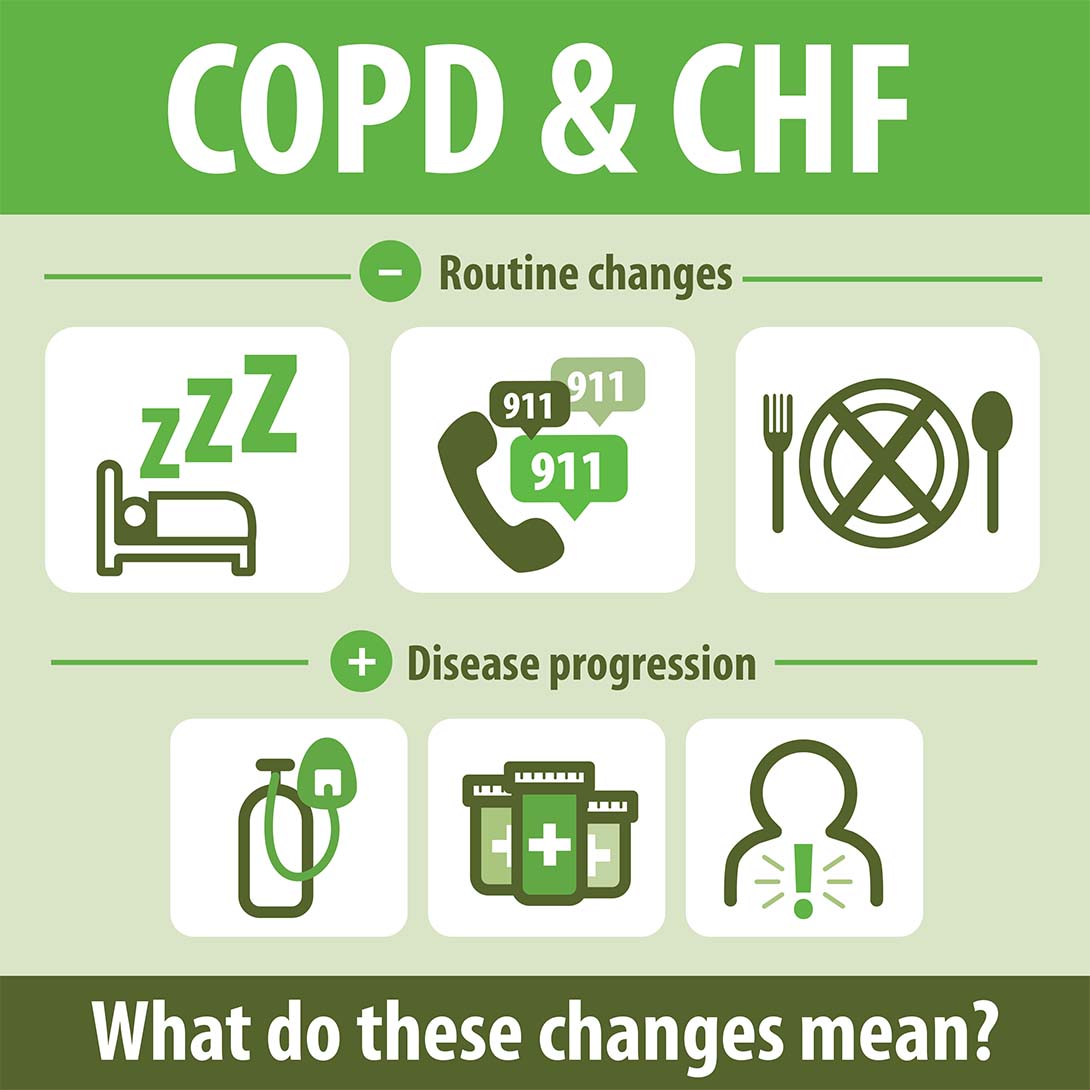
Beyond Cancer
While palliative care probably is most closely associated with cancer patients, there are many other serious conditions that can be eased by palliative care. For example, recent studies have shown palliative care can be extremely beneficial for patients with heart disease, stroke and dementia.
It’s important for patients with serious illnesses – even if they don’t involve a malignant illness – to be aware that palliative care support is available, even if they feel their symptoms aren’t urgent enough to warrant it.

True Palliative Care
Unfortunately, palliative care often has been tied inextricably to end-of-life, says Dr. Ihrig. The fact is, palliative care specialists can be instrumental in helping patients live their lives to the fullest extent possible.
In a true palliative care model, patients work together with a medical team, including a physician, nurse practitioner and medical social worker to address the total needs of the patient and family – including issues that may be not only physical in nature, but also psychological, social, emotional, or behavioral.
“Palliative care is about living,” explains Dr. Ihrig.
The most important thing is that physicians should be fully transparent with their patients in regard to information about their prognosis and treatment options, and then work closely with them to help them identify what is most important to them so they can help them achieve their most important goals.
For more information on the benefits of palliative care, please call us at 1-888-564-3405.
If you found this information helpful, please share it with your network and community.
Copyright © 2018 Crossroads Hospice. All rights reserved.